With the rapid spread of COVID-19 all over the World, people have been ordered to stay at home and avoid engaging in non- essential activities. For people living with a disability, especially for the most vulnerable, being told to isolate and stay indoors may mean spending longer periods of time lying in bed. Whilst this may seem to be a safe, comfortable place for these individuals, long periods of time in bed can lead to life threatening complications. The dangers associated with pressure injury are well documented, however there is one often overlooked area and that is the one we are particularly concerned with and very passionate about… that is the impact on posture!
essential activities. For people living with a disability, especially for the most vulnerable, being told to isolate and stay indoors may mean spending longer periods of time lying in bed. Whilst this may seem to be a safe, comfortable place for these individuals, long periods of time in bed can lead to life threatening complications. The dangers associated with pressure injury are well documented, however there is one often overlooked area and that is the one we are particularly concerned with and very passionate about… that is the impact on posture!
Good posture is essential for function, not just to allow an individual to sustain their body against gravity in order to engage in meaningful activities, but also physiological function of the body, such as respiration, circulation, digestion, and bowel and bladder motion. The better the posture, the higher the degree of muscular efficiency.
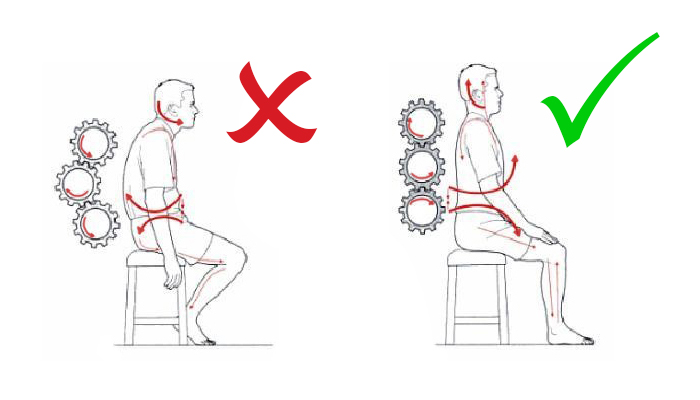
We know that gravity, asymmetric postures and time spent in a harmful position can lead to pain, discomfort, and ultimately tissue adaptation. Plasticity and the viscoelastic behaviour of the musculoskeletal tissue occurs when the human body or its individual body parts, remodel in adapting to a new environment. That’s why people with movement disorders, regardless of their age or condition, are at a higher risk of body shape changes with possible life-threatening consequences including:
- Increased pain and discomfort
- Skin integrity issues
- Orthopedic deformity and muscle shortening – immobility
- Poor systemic function – respiratory problems, bladder and bowel difficulties
- Sleeping, communication, and feeding difficulties
- Lack of stability and balance – leads to poor seating tolerance and decrease of function
- Side effects and impact on thermoregulation
- Increase handling and personal care from caregivers
In 2018, a group of researchers (Ágústsson, A.; Sveinsson, T.; Pope, P. & Rodby-Bousquet) wanted to analyse the association between the preferred posture for lying and the odds of developing scoliosis and windswept hips in adults with cerebral palsy. The sample comprised of 830 adults (469 male and 361 female) with cerebral palsy, their ages ranged from 16 to 73 years old, and their GMFCS varied from level I to level V. Their findings showed that…
- 25% of the sample only used one position when lying in bed
- The preferred habitual posture observed in immobile adults with cerebral palsy leads to an established distortion of their body shape
- Spending more than 8 hours daily in the same lying position increased the odds of having scoliosis and windswept hips, while lying solely in a supine position, resulted in higher odds of windswept hips.
Lying and sitting are inextricably linked and failing to protect body shape in lying will invariably have an impact in sitting. Analysing postures also involves analysing the environments where those postures are sustained. Are they safe? Do they provide enough support and postural stability for sustaining that posture for quite some time? What kind of supports do we need to introduce, to make sure we prevent body shape changes?
In ordinary situations, we spend 8h a night in bed, and in that time, we twist and fidget several times. People with movement disorders tend to spend not only more time in bed during the night, but also during the day. These unprecedent times we live in right now, may increase those hours. We can look at this time as simply a collateral effect and observe people having their body shape deteriorate, OR we can use this time to promote therapeutic positioning by allowing the individual to rest comfortably while their body is being protected from postural asymmetries!

There are many informal items in the household that can be used for a start, to promote symmetry and good postural alignment. Until people are permitted to visit their Occupational Therapist or Physiotherapist and ask for an individualised professional advice, things that can be used include pillows of different shapes, densities, and materials, and rolls, blankets, or towels. There are also telehealth services available that can be used to weigh up the risk of no support while you wait to see a therapist.
It is important that you know there are several certified systems in the market that have been designed to be used in bed for a more effective and long-term use. Depending on individual needs, they can provide more or less support, can allow for more or less immersion, have different shapes depending on the area of the body that is going to be used to support, and can be made out of fibre, micro-beans, padded brackets, or mouldable components. What they all have in common is the ability to provide a gentle, comfortable, and supportive environment that ultimately will promote good postural alignment and prevent changes in body shape.
Medifab is happy to support you or someone you know that may need our help! We provide clinical training to healthcare professionals and product support for families and end-users. Please get in touch with us either by emailing us at [email protected] or ring our head office as ask for the Clinical Team at 0800 543 343 (New Zealand) and 1300 543 343 (Australia). If face to face support is required, please get in touch with us and we can offer our telehealth service to support you!
Ágústsson, A. & Sveinsson, T. & Pope, P. & Rodby-Bousquet, E. (2018) Preferred posture in lying and its association with scoliosis and windswept hips in adults with cerebral palsy. Disability and Rehabilitation. 1-5.
Carter B. (2017) The Conversation, online newsletter. Poor posture in people with disabilities can be fatal. https://theconversation.com/poor-posture-in-people-with-disabilities-can…
Crawford S. & Stinson M. (2015) Management of 24hr-Body Positioning. In: International Handbook of Occupational Therapy Interventions. (Ed. Söderback, I). 189-203. Springer.
Hill, S., Goldsmith, J. (2010) Biomechanics and Prevention of Body Shape Distortion. The Tizard Learning Disability Review. 15(2):15-29.
Humphreys G., King T., Jex J., Rogers M., Blake S., Thompson-Coon J., et al. (2019) Sleep positioning systems for children and adults with a neurodisability: A systematic review. Br J Occup Ther.82(1):5–14
Gough, M. (2009) Continuous postural management and the prevention of deformity in children with cerebral palsy: an appraisal. Developmental Medicine and Child Neurology. 51: p. 105-110.
Owens K, Gemma D. (2017) A study into the effectiveness of 24-Hour Postural Care in the Management of Contractures in Care Homes. Middlesbrough Council.
Pope PM. (2007) Severe and complex neurological disability: management of the physical condition. Edinburgh: Butterworth-Heinemann/Elsevier.
Waugh A, Hill S. (2009) Body shape distortion: promoting postural care at night. Learning Disability Practice. Vol 12 ( 7) ; 25-29






 to prevent body shape changes but also to prevent for skin breakdown. It is important that supine lying is symmetrical and is sustained for as long as possible. That means that if in order to keep pelvis and shoulders aligned you need support from external elements, then introduce them! This intervention needs to be gentle by supporting both sides of the pelvis and trunk with support at the hips towards the midline. That may also require a support under the knees and/or lateral supports to avoid collapsing to the sides. Ensure that the feet are also supported and watch out for increased pressure at the heels.
to prevent body shape changes but also to prevent for skin breakdown. It is important that supine lying is symmetrical and is sustained for as long as possible. That means that if in order to keep pelvis and shoulders aligned you need support from external elements, then introduce them! This intervention needs to be gentle by supporting both sides of the pelvis and trunk with support at the hips towards the midline. That may also require a support under the knees and/or lateral supports to avoid collapsing to the sides. Ensure that the feet are also supported and watch out for increased pressure at the heels.






